Table of Contents
Introduction
When people talk about fertility, the conversation often focuses on women. Yet, male fertility plays an equal role in conception, contributing to nearly 50% of infertility issues worldwide. Most people think a simple sperm count test is enough to assess male fertility, but there’s much more to the story.
In this blog, we dive deeper into the lesser-known aspects of male reproductive health. From sperm motility to morphology, DNA quality, hormones, and lifestyle factors, we explore what truly matters when evaluating male fertility.
1. The Myth of Sperm Count Being Everything
Sperm count refers to the number of sperm present in one millilitre of semen. While it is an important factor, it’s not the only one:
-
- A man can have a normal sperm count but still be infertile.
-
- Conversely, some men with low sperm count may still be able to conceive naturally.
So, relying solely on sperm count gives an incomplete picture. It’s like evaluating a car by how much fuel is in the tank, without checking the engine or tyres.
2. Key Parameters That Matter in Male Fertility
a) Sperm Motility (Movement)
-
- This refers to how well sperm swim toward the egg.
-
- Progressive motility (forward movement) is crucial for natural conception.
-
- Poor motility means sperm may not reach the egg, even if the count is high.
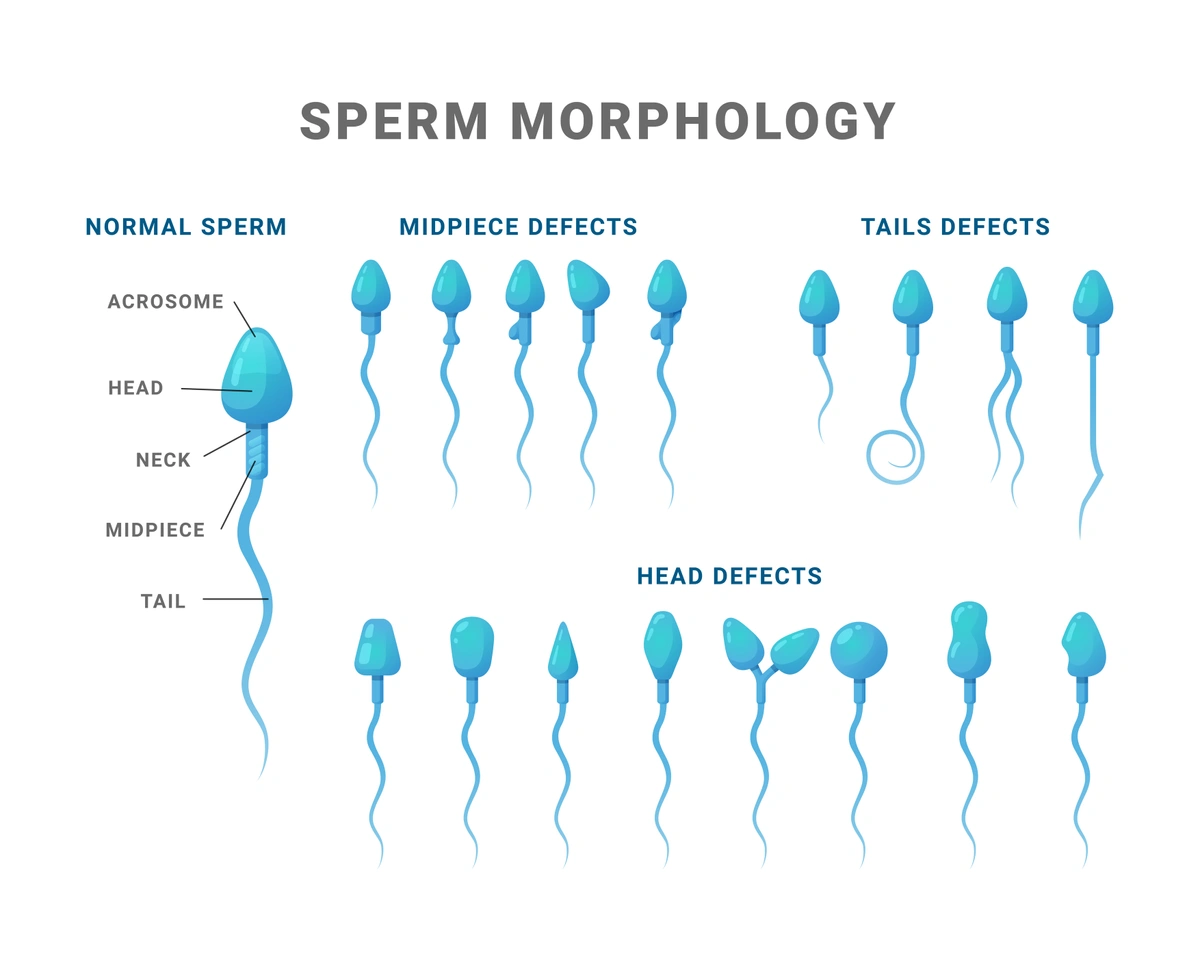
b) Sperm Morphology (Shape and Structure)
-
- Healthy sperm have an oval head, a midpiece, and a tail.
-
- Abnormal morphology (misshapen sperm) can reduce the chances of fertilisation.
-
- According to WHO, even 4% normal-shaped sperm can be considered fertile — quality matters more than quantity.
c) Sperm DNA Fragmentation
-
- This measures the integrity of the sperm’s genetic material.
-
- High DNA fragmentation can result in failed fertilisation, poor embryo development, or early miscarriage.
-
- Causes include oxidative stress, smoking, infection, and advanced age.
d) Semen Volume and pH
-
- Semen provides the medium in which sperm travel.
-
- Very low semen volume or abnormal pH levels may indicate infections or glandular problems.
e) Hormonal Profile
-
- Testosterone, FSH, LH, and prolactin are essential hormones for sperm production.
- Imbalances in these hormones may point to underlying endocrine disorders.
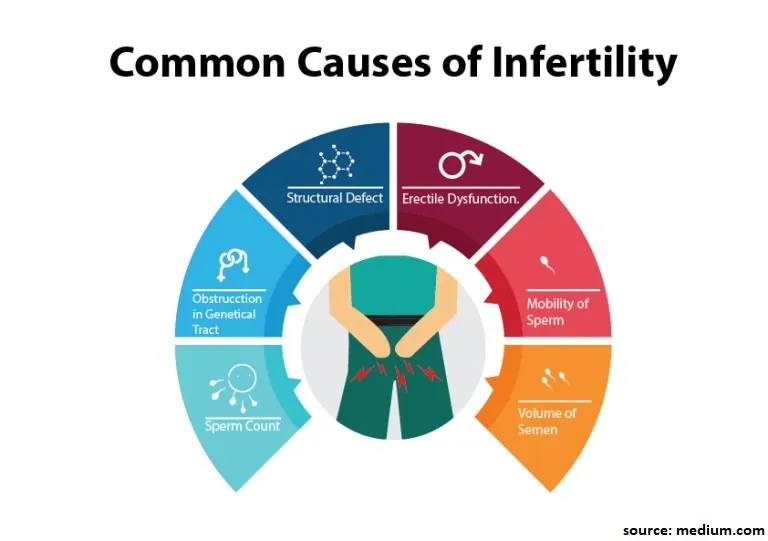
3. Common Causes of Male Fertility Problems
a) Lifestyle Factors
-
- Smoking, alcohol, and drug use
-
- Obesity and poor diet
-
- Sedentary lifestyle and prolonged heat exposure (e.g., hot laptops on lap)
-
- Stress and poor sleep quality
b) Environmental Toxins
-
- Air pollution and heavy metals
-
- Plastics (BPA), pesticides, and industrial chemicals
-
- These act as endocrine disruptors that impair sperm health
c) Medical Conditions
-
- Varicocele (enlarged veins in the scrotum)
-
- Undescended testicles
-
- Infections like mumps, STIs, or prostatitis
-
- Chronic illnesses such as diabetes or thyroid disorders
d) Genetic Causes
-
- Klinefelter syndrome, Y chromosome microdeletions
- Genetic abnormalities may reduce or eliminate sperm production
4. How Is Male Fertility Tested?
a) Semen Analysis
-
- This is the basic test that evaluates count, motility, morphology, and volume.
-
- It is best done after 2-3 days of abstinence.
b) Advanced Sperm Function Tests
-
- DNA Fragmentation Index (DFI)
-
- Vitality testing
c) Hormone Testing
-
- Blood tests to check FSH, LH, testosterone, and prolactin levels
d) Scrotal Ultrasound
-
- Helps detect varicocele, blockages, or structural problems
e) Genetic Testing
-
- Karyotype and Y chromosome micro deletion testing is recommended if sperm count is extremely low or zero
5. Male Fertility and Age: Does It Matter?
Unlike women, men remain fertile much longer, but fertility does decline with age:
-
- Sperm quality begins to reduce after age 40
-
- Increased risk of genetic mutations and poor embryo quality
-
- Higher chances of miscarriage or disorders in offspring
Men planning to delay fatherhood may consider sperm banking in their 30s.
6. How to Improve Male Fertility Naturally
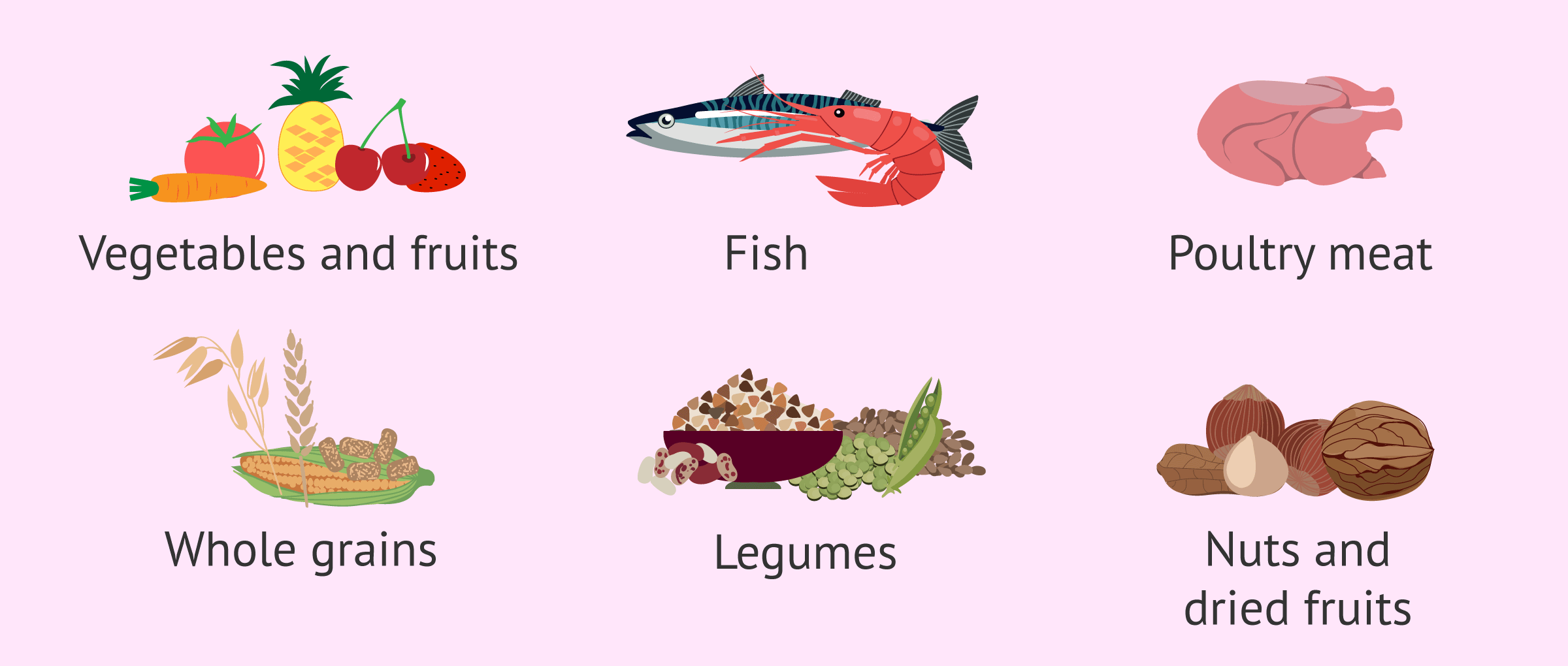
a) Nutrition
-
- Eat antioxidant-rich foods: berries, nuts, seeds, leafy greens
-
- Supplements: Zinc, Vitamin C, Vitamin E, CoQ10, Omega-3
b) Exercise and Weight Management
-
- Regular physical activity boosts testosterone and improves blood flow
c) Avoid Heat and Radiation Exposure
-
- No tight underwear, prolonged hot baths, or placing laptops on the lap
d) Quit Smoking, Limit Alcohol, Avoid Drugs
-
- All three significantly impair sperm quality and hormone balance
e) Manage Stress
-
- Chronic stress leads to hormonal imbalances
- Techniques: yoga, meditation, therapy, or time off screens
7. When to Seek Medical Help
Couples should seek evaluation if:
-
- They’ve been trying to conceive for over a year (or 6 months if over 35)
-
- There is a known history of reproductive or sexual health problems
-
- The male partner has undergone chemotherapy, radiation, or major surgery
Conclusion
Male fertility is complex, and sperm count is just one piece of a much larger puzzle. Motility, morphology, DNA quality, and lifestyle factors play an equally important role in determining reproductive potential.
At a time when infertility is rising — especially in urban India — awareness is power. Understanding what truly matters in male fertility can help couples act early, make better decisions, and explore solutions with empathy and science. Whether it’s through lifestyle changes or assisted reproductive techniques, help is available — and it begins with the right knowledge.